Unlocking Stroke Severity: NIH Stroke Scale Score of 14
Discover the significance of NIH Stroke Scale score of 14 in assessing stroke severity. Gain insights to optimize patient care and enhance outcomes.
In the realm of healthcare, the NIH Stroke Scale score of 14 emerges as a critical metric, often serving as a pivotal indicator in assessing the severity and prognosis of stroke patients. With strokes posing a significant health concern globally, understanding and interpreting this numerical measure becomes paramount in guiding treatment strategies and prognosticating patient outcomes. In this article, we delve into the intricacies of the NIH Stroke Scale score of 14, exploring its clinical significance, implications for patient care, and the broader landscape of stroke management. Through comprehensive analysis and expert insights, we aim to elucidate the complexities surrounding this vital healthcare parameter, empowering healthcare professionals and stakeholders with actionable knowledge to optimize stroke management protocols and enhance patient outcomes.
Top 10 Points about NIH Stroke Scale score of 14 :
- Introduction to NIH Stroke Scale
- Understanding Stroke Severity
- Role of NIH Stroke Scale Score of 14
- Interpreting NIH Stroke Scale Scores
- Diagnostic Importance in Healthcare
- Treatment Implications for Score of 14
- Prognosticating Patient Outcomes
- NIH Stroke Scale in Clinical Practice
- Challenges and Considerations
- Future Directions in Stroke Management
Several facts about NIH Stroke Scale score of 14
Introduction to NIH Stroke Scale
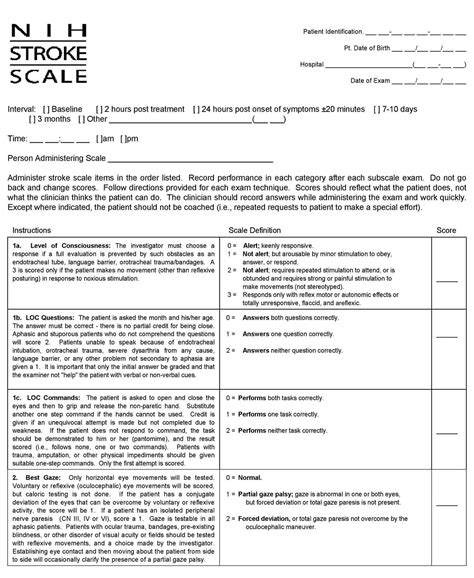
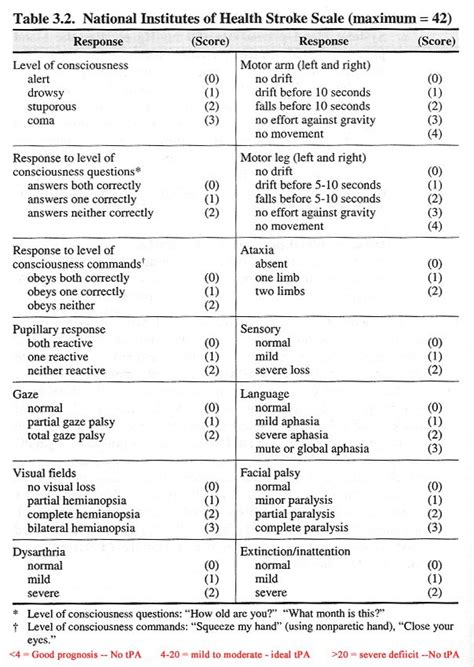
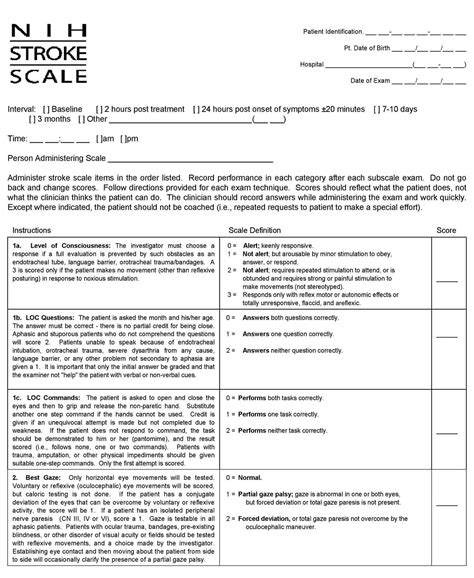
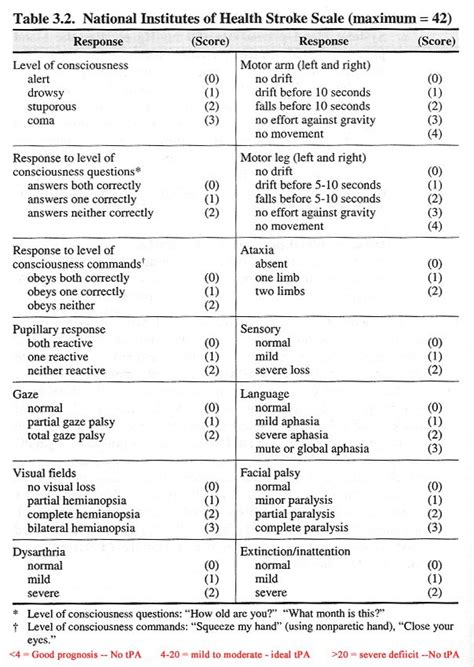
Understanding the complexities of stroke severity assessment is crucial in healthcare. One of the primary tools used for this purpose is the NIH Stroke Scale (NIHSS), which offers a standardized method to evaluate the extent of neurological deficit in stroke patients. The scale comprises various components, each assessing different aspects of neurological function such as consciousness, motor function, language, and sensory function.

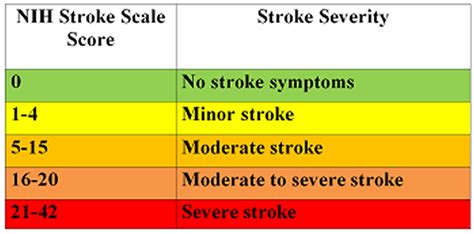
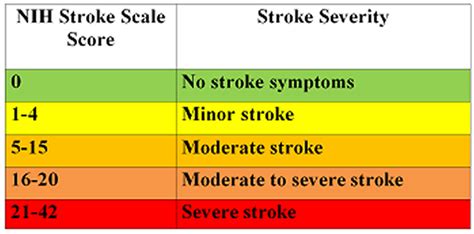
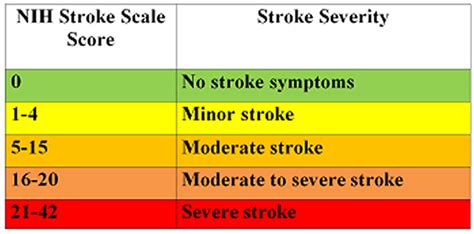
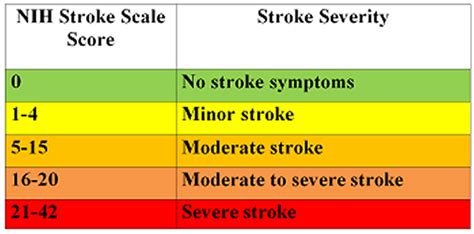
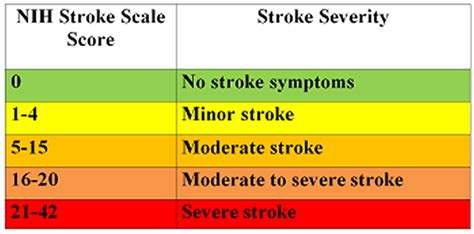
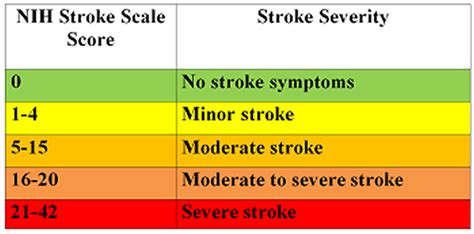
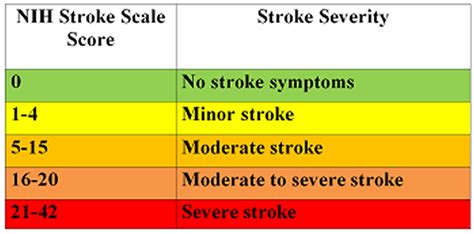
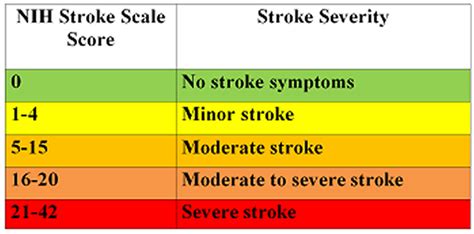
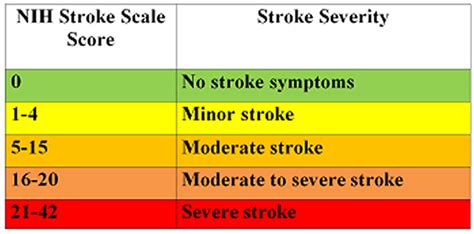
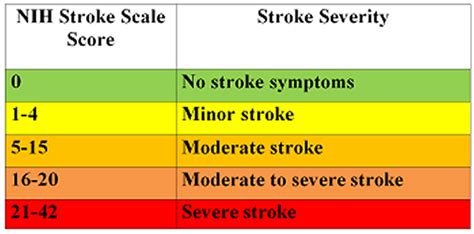
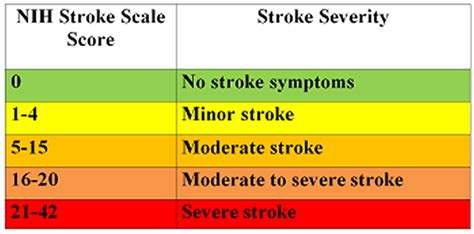
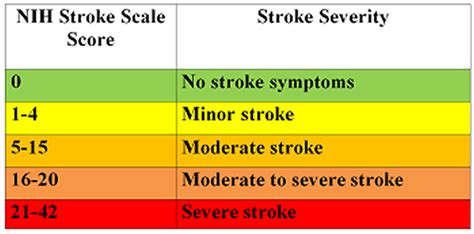
Understanding Stroke Severity
Stroke, a leading cause of disability and mortality worldwide, encompasses a spectrum of severity ranging from mild to severe. Severity assessment is pivotal in determining the appropriate treatment and predicting patient outcomes. The NIH Stroke Scale plays a crucial role in this process, offering a quantitative measure to gauge the extent of neurological impairment following a stroke. A score of 14 on the NIHSS indicates a moderate degree of stroke severity.

Role of NIH Stroke Scale Score of 14
The NIH Stroke Scale score of 14 holds significant clinical relevance, indicating a moderate neurological deficit in stroke patients. Healthcare providers utilize this score to guide treatment decisions, assess the need for interventions such as thrombolysis or mechanical thrombectomy, and prognosticate patient outcomes. A thorough understanding of the implications associated with an NIHSS score of 14 is essential for optimizing patient care and improving outcomes.

Interpreting NIH Stroke Scale Scores
Interpretation of NIH Stroke Scale scores requires careful consideration of various factors, including the specific components contributing to the score and the individual patient's clinical presentation. A score of 14 may indicate impairments in motor function, sensation, language, and other neurological domains. Healthcare providers must integrate this information with other clinical data to formulate an accurate assessment and treatment plan tailored to the patient's needs.
Diagnostic Importance in Healthcare
The NIH Stroke Scale serves as a valuable diagnostic tool in healthcare, aiding clinicians in identifying and characterizing strokes. A score of 14 on the NIHSS suggests a moderate degree of neurological impairment, prompting further evaluation and intervention. Prompt recognition of stroke severity facilitates timely initiation of appropriate treatments, which is crucial for improving patient outcomes and reducing long-term disability.

Treatment Implications for Score of 14
For patients with an NIH Stroke Scale score of 14, treatment decisions hinge on various factors, including the time of symptom onset, presence of contraindications, and individual patient characteristics. Treatment modalities such as intravenous thrombolysis with tissue plasminogen activator (tPA) or mechanical thrombectomy may be considered depending on the clinical scenario. The goal is to restore blood flow to the affected area of the brain promptly, minimize further neurological damage, and improve overall outcomes.
Prognosticating Patient Outcomes
An NIH Stroke Scale score of 14 offers valuable prognostic information regarding patient outcomes following a stroke. While a score of 14 indicates a moderate degree of neurological deficit, individual prognosis may vary based on factors such as age, comorbidities, and response to treatment. Healthcare providers use this information to counsel patients and families, set realistic expectations, and optimize post-stroke rehabilitation plans.

NIH Stroke Scale in Clinical Practice
The NIH Stroke Scale is a cornerstone of stroke assessment in clinical practice, facilitating standardized evaluation and communication among healthcare providers. A score of 14 prompts a comprehensive assessment of neurological function, guiding the selection of appropriate interventions and monitoring of patient progress. Integration of the NIHSS into routine clinical practice enhances efficiency, accuracy, and consistency in stroke management.
Challenges and Considerations
Despite its utility, the NIH Stroke Scale is not without limitations. Interpretation of scores may be influenced by factors such as patient cooperation, examiner experience, and the presence of confounding conditions. Additionally, certain neurological deficits may not be adequately captured by the scale, leading to underestimation or overestimation of stroke severity. Healthcare providers must be aware of these challenges and exercise clinical judgment when interpreting NIHSS scores to ensure optimal patient care.

Future Directions in Stroke Management
Ongoing research endeavors aim to enhance stroke management strategies, including the refinement of assessment tools such as the NIH Stroke Scale. Advancements in neuroimaging, biomarkers, and telemedicine hold promise for improving stroke diagnosis, treatment selection, and monitoring of patient progress. As our understanding of stroke pathophysiology evolves, so too will our approaches to stroke management, with the ultimate goal of reducing the burden of stroke-related disability and mortality.
Sources: NIH Stroke Scale Handbook, American Stroke Association Guidelines
NIH Stroke Scale score of 14 in Professional's eye
In the realm of healthcare, the
NIH Stroke Scale score of 14 emerges as a pivotal indicator in assessing the severity and prognosis of stroke patients. This standardized tool, developed by the National Institutes of Health, offers healthcare professionals a structured approach to evaluating neurological deficits following a stroke. The scale encompasses various components, each assessing specific aspects of neurological function such as consciousness, motor function, language, and sensory function. Upon admission to a healthcare facility, stroke patients undergo a comprehensive neurological assessment, which often includes the administration of the NIH Stroke Scale. The score derived from this assessment provides valuable insights into the extent of neurological impairment, guiding treatment decisions and prognosticating patient outcomes. A score of
14 on the NIH Stroke Scale indicates a moderate degree of stroke severity, prompting healthcare providers to initiate timely interventions to mitigate further neurological damage and optimize recovery. Transitioning from assessment to intervention, healthcare teams collaborate to tailor treatment plans to address the individual needs and circumstances of each patient. Imaging studies, such as computed tomography (CT) scans or magnetic resonance imaging (MRI), may complement the clinical assessment, aiding in the localization and characterization of the stroke lesion. Through a multidisciplinary approach, encompassing neurology, emergency medicine, rehabilitation, and other specialties, healthcare professionals strive to deliver comprehensive care to stroke patients, with the overarching goal of minimizing disability and maximizing quality of life.

Transitioning from assessment to intervention, healthcare teams collaborate to tailor treatment plans to address the individual needs and circumstances of each patient. Imaging studies, such as computed tomography (CT) scans or magnetic resonance imaging (MRI), may complement the clinical assessment, aiding in the localization and characterization of the stroke lesion. Through a multidisciplinary approach, encompassing neurology, emergency medicine, rehabilitation, and other specialties, healthcare professionals strive to deliver comprehensive care to stroke patients, with the overarching goal of minimizing disability and maximizing quality of life.

Timely interventions are paramount in the management of stroke, particularly in cases where the NIH Stroke Scale score indicates moderate severity. For patients with an NIHSS score of
14, treatment decisions may include the administration of intravenous thrombolysis with tissue plasminogen activator (tPA) within the established time window, typically up to 4.5 hours from symptom onset. In select cases, mechanical thrombectomy, a procedure involving the removal of a blood clot from the cerebral vasculature, may be indicated to restore blood flow to the affected area of the brain. The decision to pursue these interventions necessitates a careful assessment of the potential risks and benefits, taking into account factors such as the patient's age, comorbidities, and contraindications to treatment. Healthcare providers must also consider the availability of specialized resources and expertise, as well as the patient's preferences and goals of care, when formulating a treatment plan.
Following the acute phase of stroke management, attention shifts towards rehabilitation and secondary prevention strategies. Stroke survivors may experience a range of physical, cognitive, and emotional challenges, necessitating a coordinated approach to post-stroke care. Rehabilitation services, including physical therapy, occupational therapy, and speech therapy, play a vital role in promoting recovery and facilitating optimal functioning. The implementation of secondary prevention measures, such as antithrombotic therapy, statin therapy, blood pressure management, and lifestyle modifications, aims to reduce the risk of recurrent stroke and improve long-term outcomes. Education and support for patients and caregivers are integral components of stroke care, empowering individuals to navigate the complexities of stroke recovery and make informed decisions regarding their health and well-being.
As healthcare systems evolve, efforts to enhance stroke care continue to evolve, with a focus on optimizing outcomes and promoting health equity. Advances in telemedicine technologies hold promise for expanding access to specialized stroke care, particularly in rural and underserved communities. Telestroke networks enable remote consultation and decision-making, facilitating timely access to stroke expertise and interventions. Furthermore, ongoing research endeavors seek to improve our understanding of stroke pathophysiology, identify novel therapeutic targets, and refine existing treatment modalities. Collaborative initiatives, involving healthcare providers, researchers, policymakers, and advocacy organizations, are essential for driving innovation and fostering improvements in stroke care delivery. By leveraging collective expertise and resources, we can strive towards a future where all individuals affected by stroke receive timely, comprehensive, and compassionate care, regardless of geographic location or socioeconomic status.
In conclusion, the
NIH Stroke Scale score of 14 serves as a critical tool in the assessment and management of stroke, guiding treatment decisions and prognosticating patient outcomes. Timely interventions, informed by a comprehensive understanding of stroke severity and individual patient characteristics, are essential for optimizing recovery and minimizing disability. A collaborative approach, involving healthcare providers, patients, caregivers, and community stakeholders, is paramount in addressing the complex needs of stroke survivors and promoting long-term well-being. As we continue to advance our knowledge and capabilities in stroke care, our collective efforts will pave the way for improved outcomes and a brighter future for individuals affected by stroke.
Sources:National Institutes of Health Stroke Scale HandbookAmerican Stroke Association Guidelines
Point of Views : NIH Stroke Scale score of 14
Assessment Tool: The
NIH Stroke Scale score of 14 serves as a standardized assessment tool utilized by healthcare professionals to evaluate the severity of neurological deficits in stroke patients.
Quantitative Measure: With its structured approach, the NIH Stroke Scale offers a quantitative measure of neurological impairment, aiding in treatment decision-making and prognostication.
Multi-dimensional Evaluation: The scale encompasses various components, including consciousness, motor function, language, and sensory function, providing a comprehensive evaluation of the patient's neurological status.
Severity Indicator: A score of
14 on the NIH Stroke Scale signifies a moderate degree of stroke severity, prompting healthcare providers to initiate timely interventions to mitigate further neurological damage.
Treatment Guidance: Healthcare teams use the NIHSS score of
14 to guide treatment decisions, such as the administration of thrombolytic therapy or mechanical thrombectomy, tailored to the individual patient's needs.
Prognostic Value: The NIH Stroke Scale score of
14 offers valuable prognostic information regarding patient outcomes, enabling healthcare providers to counsel patients and families and optimize post-stroke rehabilitation plans.
Standardized Approach: By providing a standardized approach to stroke assessment, the NIH Stroke Scale facilitates consistent communication and decision-making among healthcare providers, promoting efficient and effective stroke care.
Continued Research: Ongoing research endeavors seek to enhance our understanding of stroke pathophysiology and refine assessment tools such as the NIH Stroke Scale, with the ultimate goal of improving outcomes for stroke patients.
Conclusion :As we conclude our exploration of the NIH Stroke Scale score of 14 and its significance in stroke assessment, it is evident that this standardized tool plays a crucial role in guiding healthcare professionals in their management of stroke patients. Through its multi-dimensional evaluation of neurological deficits, the NIH Stroke Scale provides a quantitative measure of stroke severity, enabling timely interventions to mitigate further neurological damage and optimize patient outcomes. Whether it be initiating thrombolytic therapy or facilitating rehabilitation plans, the NIH Stroke Scale score of 14 serves as a valuable guidepost in the complex landscape of stroke care.
As healthcare providers, researchers, and policymakers continue to advance our understanding of stroke pathophysiology and refine assessment tools, such as the NIH Stroke Scale, we can expect further improvements in stroke management and outcomes. It is imperative that we remain vigilant in our efforts to optimize stroke care delivery, leveraging evidence-based practices and collaborative approaches to ensure that all individuals affected by stroke receive the comprehensive and compassionate care they deserve. Together, let us continue to strive towards a future where strokes are promptly recognized, effectively treated, and their impact minimized, ultimately improving the quality of life for stroke survivors and their families.
Questions and Answer for NIH Stroke Scale score of 14
When exploring the topic of NIH Stroke Scale score of 14, individuals often have several questions. Below are some common inquiries along with their corresponding answers:
- 1. What does a NIH Stroke Scale score of 14 indicate?
The NIH Stroke Scale score of 14 indicates a moderate degree of neurological deficit in stroke patients. It serves as a standardized tool used by healthcare professionals to evaluate various aspects of neurological function, including consciousness, motor function, language, and sensory function.
- 2. What treatment options are available for a NIH Stroke Scale score of 14?
For patients with a NIH Stroke Scale score of 14, treatment options may include intravenous thrombolysis with tissue plasminogen activator (tPA) within the established time window or mechanical thrombectomy to restore blood flow to the affected area of the brain. Treatment decisions are based on factors such as the time of symptom onset, patient characteristics, and the presence of contraindications.
- 3. What is the prognosis for a NIH Stroke Scale score of 14?
The prognosis for a NIH Stroke Scale score of 14 varies depending on factors such as the individual patient's age, comorbidities, response to treatment, and rehabilitation potential. While a score of 14 indicates a moderate degree of stroke severity, timely interventions and comprehensive rehabilitation can help improve outcomes and minimize long-term disability.
- 4. How is the NIH Stroke Scale score of 14 assessed?
The NIH Stroke Scale score of 14 is assessed through a comprehensive neurological evaluation conducted by trained healthcare professionals. This evaluation involves assessing the patient's level of consciousness, motor function, language skills, and sensory function, with each component contributing to the overall score.
Label :NIH Stroke Scale, Severity Assessment, Treatment Options, Prognosis
Keyword : NIH Stroke Scale score of 14
Discover the significance of NIH Stroke Scale score of 14 in assessing stroke severity. Gain insights to optimize patient care and enhance outcomes.
In the realm of healthcare, the NIH Stroke Scale score of 14 emerges as a critical metric, often serving as a pivotal indicator in assessing the severity and prognosis of stroke patients. With strokes posing a significant health concern globally, understanding and interpreting this numerical measure becomes paramount in guiding treatment strategies and prognosticating patient outcomes. In this article, we delve into the intricacies of the NIH Stroke Scale score of 14, exploring its clinical significance, implications for patient care, and the broader landscape of stroke management. Through comprehensive analysis and expert insights, we aim to elucidate the complexities surrounding this vital healthcare parameter, empowering healthcare professionals and stakeholders with actionable knowledge to optimize stroke management protocols and enhance patient outcomes.
Top 10 Points about NIH Stroke Scale score of 14 :
- Introduction to NIH Stroke Scale
- Understanding Stroke Severity
- Role of NIH Stroke Scale Score of 14
- Interpreting NIH Stroke Scale Scores
- Diagnostic Importance in Healthcare
- Treatment Implications for Score of 14
- Prognosticating Patient Outcomes
- NIH Stroke Scale in Clinical Practice
- Challenges and Considerations
- Future Directions in Stroke Management
Several facts about NIH Stroke Scale score of 14
Introduction to NIH Stroke Scale
Understanding the complexities of stroke severity assessment is crucial in healthcare. One of the primary tools used for this purpose is the NIH Stroke Scale (NIHSS), which offers a standardized method to evaluate the extent of neurological deficit in stroke patients. The scale comprises various components, each assessing different aspects of neurological function such as consciousness, motor function, language, and sensory function.

Understanding Stroke Severity
Stroke, a leading cause of disability and mortality worldwide, encompasses a spectrum of severity ranging from mild to severe. Severity assessment is pivotal in determining the appropriate treatment and predicting patient outcomes. The NIH Stroke Scale plays a crucial role in this process, offering a quantitative measure to gauge the extent of neurological impairment following a stroke. A score of 14 on the NIHSS indicates a moderate degree of stroke severity.

Role of NIH Stroke Scale Score of 14
The NIH Stroke Scale score of 14 holds significant clinical relevance, indicating a moderate neurological deficit in stroke patients. Healthcare providers utilize this score to guide treatment decisions, assess the need for interventions such as thrombolysis or mechanical thrombectomy, and prognosticate patient outcomes. A thorough understanding of the implications associated with an NIHSS score of 14 is essential for optimizing patient care and improving outcomes.

Interpreting NIH Stroke Scale Scores
Interpretation of NIH Stroke Scale scores requires careful consideration of various factors, including the specific components contributing to the score and the individual patient's clinical presentation. A score of 14 may indicate impairments in motor function, sensation, language, and other neurological domains. Healthcare providers must integrate this information with other clinical data to formulate an accurate assessment and treatment plan tailored to the patient's needs.
Diagnostic Importance in Healthcare
The NIH Stroke Scale serves as a valuable diagnostic tool in healthcare, aiding clinicians in identifying and characterizing strokes. A score of 14 on the NIHSS suggests a moderate degree of neurological impairment, prompting further evaluation and intervention. Prompt recognition of stroke severity facilitates timely initiation of appropriate treatments, which is crucial for improving patient outcomes and reducing long-term disability.

Treatment Implications for Score of 14
For patients with an NIH Stroke Scale score of 14, treatment decisions hinge on various factors, including the time of symptom onset, presence of contraindications, and individual patient characteristics. Treatment modalities such as intravenous thrombolysis with tissue plasminogen activator (tPA) or mechanical thrombectomy may be considered depending on the clinical scenario. The goal is to restore blood flow to the affected area of the brain promptly, minimize further neurological damage, and improve overall outcomes.
Prognosticating Patient Outcomes
An NIH Stroke Scale score of 14 offers valuable prognostic information regarding patient outcomes following a stroke. While a score of 14 indicates a moderate degree of neurological deficit, individual prognosis may vary based on factors such as age, comorbidities, and response to treatment. Healthcare providers use this information to counsel patients and families, set realistic expectations, and optimize post-stroke rehabilitation plans.

NIH Stroke Scale in Clinical Practice
The NIH Stroke Scale is a cornerstone of stroke assessment in clinical practice, facilitating standardized evaluation and communication among healthcare providers. A score of 14 prompts a comprehensive assessment of neurological function, guiding the selection of appropriate interventions and monitoring of patient progress. Integration of the NIHSS into routine clinical practice enhances efficiency, accuracy, and consistency in stroke management.
Challenges and Considerations
Despite its utility, the NIH Stroke Scale is not without limitations. Interpretation of scores may be influenced by factors such as patient cooperation, examiner experience, and the presence of confounding conditions. Additionally, certain neurological deficits may not be adequately captured by the scale, leading to underestimation or overestimation of stroke severity. Healthcare providers must be aware of these challenges and exercise clinical judgment when interpreting NIHSS scores to ensure optimal patient care.

Future Directions in Stroke Management
Ongoing research endeavors aim to enhance stroke management strategies, including the refinement of assessment tools such as the NIH Stroke Scale. Advancements in neuroimaging, biomarkers, and telemedicine hold promise for improving stroke diagnosis, treatment selection, and monitoring of patient progress. As our understanding of stroke pathophysiology evolves, so too will our approaches to stroke management, with the ultimate goal of reducing the burden of stroke-related disability and mortality.
Sources: NIH Stroke Scale Handbook, American Stroke Association Guidelines
NIH Stroke Scale score of 14 in Professional's eye
In the realm of healthcare, the
NIH Stroke Scale score of 14 emerges as a pivotal indicator in assessing the severity and prognosis of stroke patients. This standardized tool, developed by the National Institutes of Health, offers healthcare professionals a structured approach to evaluating neurological deficits following a stroke. The scale encompasses various components, each assessing specific aspects of neurological function such as consciousness, motor function, language, and sensory function. Upon admission to a healthcare facility, stroke patients undergo a comprehensive neurological assessment, which often includes the administration of the NIH Stroke Scale. The score derived from this assessment provides valuable insights into the extent of neurological impairment, guiding treatment decisions and prognosticating patient outcomes. A score of
14 on the NIH Stroke Scale indicates a moderate degree of stroke severity, prompting healthcare providers to initiate timely interventions to mitigate further neurological damage and optimize recovery. Transitioning from assessment to intervention, healthcare teams collaborate to tailor treatment plans to address the individual needs and circumstances of each patient. Imaging studies, such as computed tomography (CT) scans or magnetic resonance imaging (MRI), may complement the clinical assessment, aiding in the localization and characterization of the stroke lesion. Through a multidisciplinary approach, encompassing neurology, emergency medicine, rehabilitation, and other specialties, healthcare professionals strive to deliver comprehensive care to stroke patients, with the overarching goal of minimizing disability and maximizing quality of life.

Transitioning from assessment to intervention, healthcare teams collaborate to tailor treatment plans to address the individual needs and circumstances of each patient. Imaging studies, such as computed tomography (CT) scans or magnetic resonance imaging (MRI), may complement the clinical assessment, aiding in the localization and characterization of the stroke lesion. Through a multidisciplinary approach, encompassing neurology, emergency medicine, rehabilitation, and other specialties, healthcare professionals strive to deliver comprehensive care to stroke patients, with the overarching goal of minimizing disability and maximizing quality of life.

Timely interventions are paramount in the management of stroke, particularly in cases where the NIH Stroke Scale score indicates moderate severity. For patients with an NIHSS score of
14, treatment decisions may include the administration of intravenous thrombolysis with tissue plasminogen activator (tPA) within the established time window, typically up to 4.5 hours from symptom onset. In select cases, mechanical thrombectomy, a procedure involving the removal of a blood clot from the cerebral vasculature, may be indicated to restore blood flow to the affected area of the brain. The decision to pursue these interventions necessitates a careful assessment of the potential risks and benefits, taking into account factors such as the patient's age, comorbidities, and contraindications to treatment. Healthcare providers must also consider the availability of specialized resources and expertise, as well as the patient's preferences and goals of care, when formulating a treatment plan.
Following the acute phase of stroke management, attention shifts towards rehabilitation and secondary prevention strategies. Stroke survivors may experience a range of physical, cognitive, and emotional challenges, necessitating a coordinated approach to post-stroke care. Rehabilitation services, including physical therapy, occupational therapy, and speech therapy, play a vital role in promoting recovery and facilitating optimal functioning. The implementation of secondary prevention measures, such as antithrombotic therapy, statin therapy, blood pressure management, and lifestyle modifications, aims to reduce the risk of recurrent stroke and improve long-term outcomes. Education and support for patients and caregivers are integral components of stroke care, empowering individuals to navigate the complexities of stroke recovery and make informed decisions regarding their health and well-being.
As healthcare systems evolve, efforts to enhance stroke care continue to evolve, with a focus on optimizing outcomes and promoting health equity. Advances in telemedicine technologies hold promise for expanding access to specialized stroke care, particularly in rural and underserved communities. Telestroke networks enable remote consultation and decision-making, facilitating timely access to stroke expertise and interventions. Furthermore, ongoing research endeavors seek to improve our understanding of stroke pathophysiology, identify novel therapeutic targets, and refine existing treatment modalities. Collaborative initiatives, involving healthcare providers, researchers, policymakers, and advocacy organizations, are essential for driving innovation and fostering improvements in stroke care delivery. By leveraging collective expertise and resources, we can strive towards a future where all individuals affected by stroke receive timely, comprehensive, and compassionate care, regardless of geographic location or socioeconomic status.
In conclusion, the
NIH Stroke Scale score of 14 serves as a critical tool in the assessment and management of stroke, guiding treatment decisions and prognosticating patient outcomes. Timely interventions, informed by a comprehensive understanding of stroke severity and individual patient characteristics, are essential for optimizing recovery and minimizing disability. A collaborative approach, involving healthcare providers, patients, caregivers, and community stakeholders, is paramount in addressing the complex needs of stroke survivors and promoting long-term well-being. As we continue to advance our knowledge and capabilities in stroke care, our collective efforts will pave the way for improved outcomes and a brighter future for individuals affected by stroke.
Sources:National Institutes of Health Stroke Scale HandbookAmerican Stroke Association Guidelines
Point of Views : NIH Stroke Scale score of 14
Assessment Tool: The
NIH Stroke Scale score of 14 serves as a standardized assessment tool utilized by healthcare professionals to evaluate the severity of neurological deficits in stroke patients.
Quantitative Measure: With its structured approach, the NIH Stroke Scale offers a quantitative measure of neurological impairment, aiding in treatment decision-making and prognostication.
Multi-dimensional Evaluation: The scale encompasses various components, including consciousness, motor function, language, and sensory function, providing a comprehensive evaluation of the patient's neurological status.
Severity Indicator: A score of
14 on the NIH Stroke Scale signifies a moderate degree of stroke severity, prompting healthcare providers to initiate timely interventions to mitigate further neurological damage.
Treatment Guidance: Healthcare teams use the NIHSS score of
14 to guide treatment decisions, such as the administration of thrombolytic therapy or mechanical thrombectomy, tailored to the individual patient's needs.
Prognostic Value: The NIH Stroke Scale score of
14 offers valuable prognostic information regarding patient outcomes, enabling healthcare providers to counsel patients and families and optimize post-stroke rehabilitation plans.
Standardized Approach: By providing a standardized approach to stroke assessment, the NIH Stroke Scale facilitates consistent communication and decision-making among healthcare providers, promoting efficient and effective stroke care.
Continued Research: Ongoing research endeavors seek to enhance our understanding of stroke pathophysiology and refine assessment tools such as the NIH Stroke Scale, with the ultimate goal of improving outcomes for stroke patients.
Conclusion :As we conclude our exploration of the NIH Stroke Scale score of 14 and its significance in stroke assessment, it is evident that this standardized tool plays a crucial role in guiding healthcare professionals in their management of stroke patients. Through its multi-dimensional evaluation of neurological deficits, the NIH Stroke Scale provides a quantitative measure of stroke severity, enabling timely interventions to mitigate further neurological damage and optimize patient outcomes. Whether it be initiating thrombolytic therapy or facilitating rehabilitation plans, the NIH Stroke Scale score of 14 serves as a valuable guidepost in the complex landscape of stroke care.
As healthcare providers, researchers, and policymakers continue to advance our understanding of stroke pathophysiology and refine assessment tools, such as the NIH Stroke Scale, we can expect further improvements in stroke management and outcomes. It is imperative that we remain vigilant in our efforts to optimize stroke care delivery, leveraging evidence-based practices and collaborative approaches to ensure that all individuals affected by stroke receive the comprehensive and compassionate care they deserve. Together, let us continue to strive towards a future where strokes are promptly recognized, effectively treated, and their impact minimized, ultimately improving the quality of life for stroke survivors and their families.
Questions and Answer for NIH Stroke Scale score of 14
When exploring the topic of NIH Stroke Scale score of 14, individuals often have several questions. Below are some common inquiries along with their corresponding answers:
- 1. What does a NIH Stroke Scale score of 14 indicate?
The NIH Stroke Scale score of 14 indicates a moderate degree of neurological deficit in stroke patients. It serves as a standardized tool used by healthcare professionals to evaluate various aspects of neurological function, including consciousness, motor function, language, and sensory function.
- 2. What treatment options are available for a NIH Stroke Scale score of 14?
For patients with a NIH Stroke Scale score of 14, treatment options may include intravenous thrombolysis with tissue plasminogen activator (tPA) within the established time window or mechanical thrombectomy to restore blood flow to the affected area of the brain. Treatment decisions are based on factors such as the time of symptom onset, patient characteristics, and the presence of contraindications.
- 3. What is the prognosis for a NIH Stroke Scale score of 14?
The prognosis for a NIH Stroke Scale score of 14 varies depending on factors such as the individual patient's age, comorbidities, response to treatment, and rehabilitation potential. While a score of 14 indicates a moderate degree of stroke severity, timely interventions and comprehensive rehabilitation can help improve outcomes and minimize long-term disability.
- 4. How is the NIH Stroke Scale score of 14 assessed?
The NIH Stroke Scale score of 14 is assessed through a comprehensive neurological evaluation conducted by trained healthcare professionals. This evaluation involves assessing the patient's level of consciousness, motor function, language skills, and sensory function, with each component contributing to the overall score.
Label :NIH Stroke Scale, Severity Assessment, Treatment Options, Prognosis
Keyword : NIH Stroke Scale score of 14
0 komentar