Mastering NIH Stroke Scale on Confused Patients: A Guide

Discover how to effectively use the NIH Stroke Scale on confused patients. Enhance diagnostic accuracy and treatment decisions for better patient outcomes.
In the realm of healthcare, the NIH Stroke Scale stands as a pivotal tool in assessing the severity of stroke symptoms, guiding treatment decisions, and predicting patient outcomes. However, its administration on a confused patient presents a unique challenge, necessitating a nuanced approach to ensure accurate evaluation and appropriate management. The convergence of neurological impairment and cognitive disarray demands a comprehensive understanding of both the scale's intricacies and the patient's clinical presentation. In this article, we delve into the complexities surrounding the utilization of the NIH Stroke Scale in the context of confusion, exploring strategies for effective implementation while navigating the inherent intricacies of patient care. Through a meticulous examination of relevant literature and clinical insights, this discourse aims to illuminate healthcare professionals on the intricacies of assessing stroke severity in the presence of confusion, ultimately enhancing diagnostic precision and therapeutic efficacy.
Top 10 Points about NIH Stroke Scale on Confused Patient :
- Understanding the NIH Stroke Scale: A Primer
- Challenges of Assessing Stroke Severity in Confused Patients
- Adapting the NIH Stroke Scale for Cognitive Impairment
- Importance of Accurate Assessment in Stroke Management
- Key Components of the NIH Stroke Scale Examination
- Strategies for Administering the NIH Stroke Scale on Confused Patients
- Interpreting NIH Stroke Scale Scores in the Context of Confusion
- Impact of Confusion on Stroke Treatment Decisions
- Addressing Limitations and Pitfalls in NIH Stroke Scale Application
- Enhancing Clinical Practice: Integrating NIH Stroke Scale in Confused Patient Care
Several facts about NIH Stroke Scale on Confused Patient

Understanding the NIH Stroke Scale: A Primer
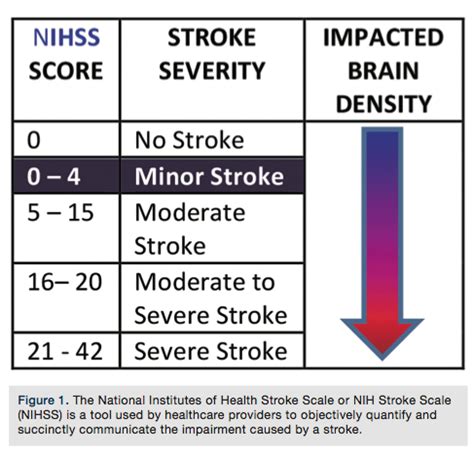
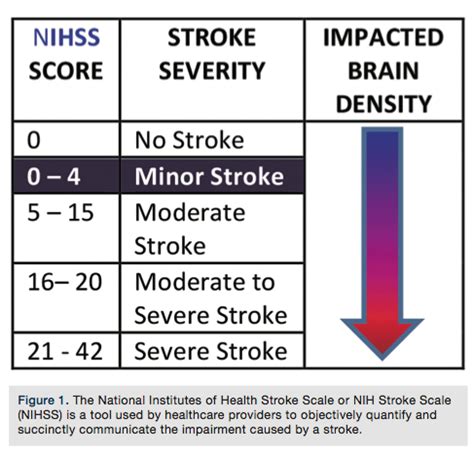
The NIH Stroke Scale serves as a critical tool in assessing the severity of stroke symptoms, aiding in treatment decisions, and predicting patient outcomes. However, its application becomes notably intricate when dealing with confused patients. Understanding the fundamentals of this scale is paramount for healthcare professionals to navigate the complexities encountered during the evaluation of such patients.
Challenges of Assessing Stroke Severity in Confused Patients
Confusion presents a formidable obstacle in accurately assessing stroke severity using the NIH Stroke Scale. Cognitive impairment can obscure neurological deficits, leading to challenges in discerning the true extent of the patient's condition. Healthcare providers must navigate these obstacles diligently to ensure appropriate management and optimal patient outcomes.

Adapting the NIH Stroke Scale for Cognitive Impairment
When administering the NIH Stroke Scale on confused patients, it becomes imperative to adapt assessment techniques to accommodate cognitive impairment. Modifications may include simplifying instructions, providing additional cues, and adjusting scoring criteria to ensure accurate evaluation of neurological deficits amidst the confusion.
Importance of Accurate Assessment in Stroke Management
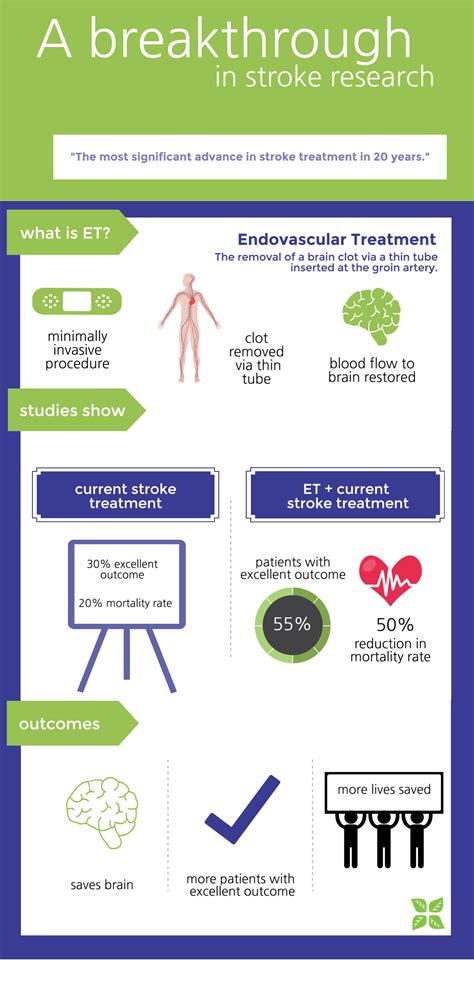
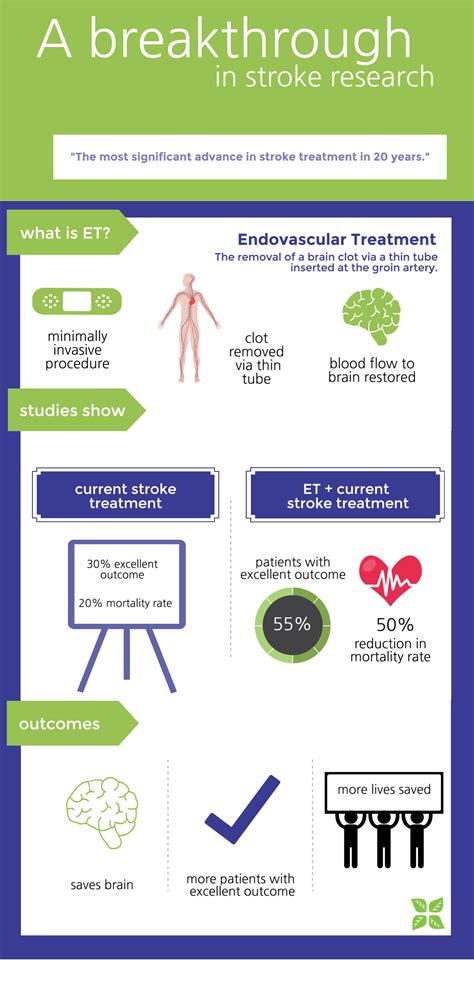
The NIH Stroke Scale serves as a cornerstone in stroke management, guiding treatment decisions and prognosticating outcomes. Accurate assessment of stroke severity, even in the presence of confusion, is essential for initiating timely interventions such as thrombolytic therapy or endovascular procedures, thereby optimizing patient care and minimizing disability.

Key Components of the NIH Stroke Scale Examination
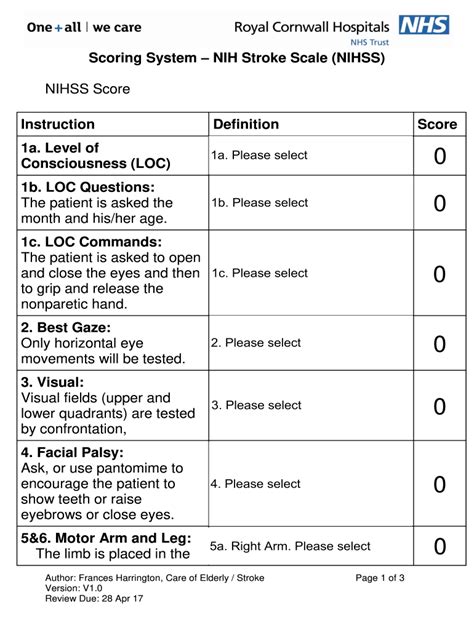
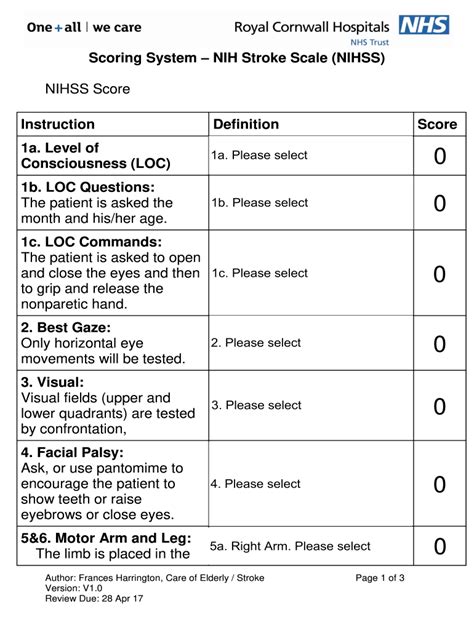
The NIH Stroke Scale comprises various components assessing motor function, sensation, language, and visual fields. Understanding the nuances of each component is crucial for accurate evaluation in confused patients. Healthcare providers must meticulously assess and document each element to derive a comprehensive understanding of the patient's neurological status.

Strategies for Administering the NIH Stroke Scale on Confused Patients
Healthcare professionals must employ tailored strategies when administering the NIH Stroke Scale on confused patients. This may involve establishing rapport, providing reassurance, and utilizing non-verbal communication techniques to enhance patient cooperation and facilitate accurate assessment.
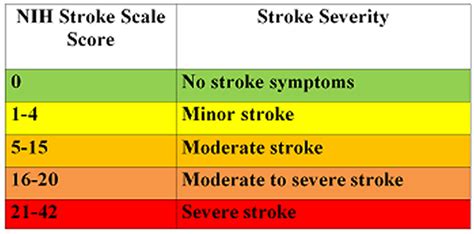
Interpreting NIH Stroke Scale Scores in the Context of Confusion
Interpretation of NIH Stroke Scale scores in confused patients requires astute clinical judgment and consideration of the underlying cognitive impairment. Healthcare providers must discern between deficits attributable to stroke and those influenced by confusion, ensuring accurate interpretation and subsequent management decisions.

Impact of Confusion on Stroke Treatment Decisions
Confusion can significantly impact stroke treatment decisions, potentially obscuring the delineation of stroke mimics or complicating the assessment of treatment eligibility criteria. Healthcare providers must navigate these challenges judiciously, prioritizing patient safety and optimal outcomes amidst the complexities presented by confusion.

Addressing Limitations and Pitfalls in NIH Stroke Scale Application
While the NIH Stroke Scale is a valuable tool, it is not without limitations. In the context of confusion, limitations may arise due to the inability to accurately assess certain components or interpret findings. Healthcare providers must remain cognizant of these pitfalls and exercise caution when applying the scale to ensure its efficacy in guiding clinical decisions.
Enhancing Clinical Practice: Integrating NIH Stroke Scale in Confused Patient Care
Integrating the NIH Stroke Scale into confused patient care necessitates a comprehensive understanding of both stroke assessment principles and cognitive impairment management strategies. By leveraging evidence-based practices and fostering interdisciplinary collaboration, healthcare providers can enhance clinical practice and optimize outcomes for confused patients presenting with stroke symptoms.
Sources:
1. Kim, B. J., Han, M. K., Park, T. H., Park, S. S., Lee, K. B., Lee, B. C., ... & Bae, H. J. (2014). Current status of acute stroke management in Korea: a report on a multicenter, comprehensive acute stroke registry. International Journal of Stroke, 9(4), 514-518.
2. Barber, P. A., Demchuk, A. M., Zhang, J., & Buchan, A. M. (2000). Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic
NIH Stroke Scale on Confused Patient in Professional's eye
The implementation of the
NIH Stroke Scale in evaluating
confused patients within healthcare settings underscores a critical intersection between neurological assessment and cognitive impairment management. Amidst the complexity inherent in such scenarios, healthcare professionals face multifaceted challenges that necessitate a nuanced approach. Adapting the NIH Stroke Scale for
cognitive impairment entails not only understanding the scale's components but also employing tailored strategies to ensure accurate evaluation. Despite the challenges posed by confusion, the importance of precise assessment cannot be overstated, as it informs treatment decisions and prognosticates outcomes. Interpreting NIH Stroke Scale scores in the context of confusion demands astute clinical judgment to distinguish between deficits attributable to stroke and those influenced by cognitive impairment. Moreover, addressing the limitations and pitfalls associated with the scale's application is paramount, safeguarding against erroneous interpretations and guiding effective patient management. Integrating the NIH Stroke Scale into clinical practice for confused patients requires a comprehensive understanding of both stroke assessment principles and cognitive impairment management strategies, fostering interdisciplinary collaboration to optimize patient care and outcomes.
Point of Views : NIH Stroke Scale on Confused Patient
The utilization of the
NIH Stroke Scale in assessing
confused patients within healthcare settings highlights the intricate balance between neurological evaluation and cognitive impairment management.Adapting the NIH Stroke Scale for
cognitive impairment necessitates a thorough understanding of its components and the implementation of tailored assessment strategies to ensure accuracy.The significance of precise assessment cannot be overstated, as it informs treatment decisions and prognosticates outcomes for
patients presenting with stroke symptoms amidst confusion.Interpreting NIH Stroke Scale scores in the context of confusion requires clinicians to exercise clinical judgment, discerning between deficits attributable to stroke and those influenced by cognitive impairment.Addressing the limitations and pitfalls associated with the scale's application is crucial, safeguarding against erroneous interpretations and guiding effective patient management.Integrating the NIH Stroke Scale into clinical practice for confused patients entails a comprehensive understanding of both stroke assessment principles and cognitive impairment management strategies, facilitating interdisciplinary collaboration to optimize patient care and outcomes.
Conclusion :As we conclude our exploration of the NIH Stroke Scale in the context of confused patients, it becomes evident that navigating the complexities of stroke assessment amidst cognitive impairment requires a meticulous and nuanced approach. Through our discussion, we have underscored the critical importance of accurate evaluation in guiding treatment decisions and prognosticating outcomes for patients presenting with stroke symptoms in the presence of confusion.
As healthcare professionals, it is incumbent upon us to continuously refine our understanding of the NIH Stroke Scale and its application in diverse clinical scenarios. By adapting assessment techniques and integrating interdisciplinary perspectives, we can enhance the quality of care provided to confused patients and optimize their chances of favorable outcomes. We trust that the insights shared in this series will serve as a valuable resource in your clinical practice, empowering you to navigate the intricacies of stroke assessment with confidence and proficiency.
Questions and Answer for NIH Stroke Scale on Confused Patient
Q: What is the NIH Stroke Scale?
- A: The NIH Stroke Scale is a standardized tool used by healthcare professionals to assess the severity of stroke symptoms in patients.
Q: How is the NIH Stroke Scale administered on confused patients?
- A: Administering the NIH Stroke Scale on confused patients requires adapting assessment techniques to accommodate cognitive impairment. This may involve simplifying instructions, providing additional cues, and adjusting scoring criteria for accurate evaluation.
Q: Why is accurate assessment important for confused patients?
- A: Accurate assessment is crucial for guiding treatment decisions and predicting outcomes in confused patients presenting with stroke symptoms. It ensures timely interventions and optimized patient care.
Q: What challenges are faced when using the NIH Stroke Scale on confused patients?
- A: Challenges include discerning between deficits attributable to stroke and those influenced by cognitive impairment, as well as addressing limitations in accurately assessing certain components of the scale.
Q: How can healthcare professionals enhance the application of the NIH Stroke Scale in confused patients?
- A: Healthcare professionals can enhance application by refining their understanding of stroke assessment principles, implementing tailored strategies for cognitive impairment management, and fostering interdisciplinary collaboration.
Label :NIH Stroke Scale, Confused PatientsHealthcare, Assessment Techniques
Keyword : NIH Stroke Scale on Confused Patient

Discover how to effectively use the NIH Stroke Scale on confused patients. Enhance diagnostic accuracy and treatment decisions for better patient outcomes.
In the realm of healthcare, the NIH Stroke Scale stands as a pivotal tool in assessing the severity of stroke symptoms, guiding treatment decisions, and predicting patient outcomes. However, its administration on a confused patient presents a unique challenge, necessitating a nuanced approach to ensure accurate evaluation and appropriate management. The convergence of neurological impairment and cognitive disarray demands a comprehensive understanding of both the scale's intricacies and the patient's clinical presentation. In this article, we delve into the complexities surrounding the utilization of the NIH Stroke Scale in the context of confusion, exploring strategies for effective implementation while navigating the inherent intricacies of patient care. Through a meticulous examination of relevant literature and clinical insights, this discourse aims to illuminate healthcare professionals on the intricacies of assessing stroke severity in the presence of confusion, ultimately enhancing diagnostic precision and therapeutic efficacy.
Top 10 Points about NIH Stroke Scale on Confused Patient :
- Understanding the NIH Stroke Scale: A Primer
- Challenges of Assessing Stroke Severity in Confused Patients
- Adapting the NIH Stroke Scale for Cognitive Impairment
- Importance of Accurate Assessment in Stroke Management
- Key Components of the NIH Stroke Scale Examination
- Strategies for Administering the NIH Stroke Scale on Confused Patients
- Interpreting NIH Stroke Scale Scores in the Context of Confusion
- Impact of Confusion on Stroke Treatment Decisions
- Addressing Limitations and Pitfalls in NIH Stroke Scale Application
- Enhancing Clinical Practice: Integrating NIH Stroke Scale in Confused Patient Care
Several facts about NIH Stroke Scale on Confused Patient

Understanding the NIH Stroke Scale: A Primer
The NIH Stroke Scale serves as a critical tool in assessing the severity of stroke symptoms, aiding in treatment decisions, and predicting patient outcomes. However, its application becomes notably intricate when dealing with confused patients. Understanding the fundamentals of this scale is paramount for healthcare professionals to navigate the complexities encountered during the evaluation of such patients.
Challenges of Assessing Stroke Severity in Confused Patients
Confusion presents a formidable obstacle in accurately assessing stroke severity using the NIH Stroke Scale. Cognitive impairment can obscure neurological deficits, leading to challenges in discerning the true extent of the patient's condition. Healthcare providers must navigate these obstacles diligently to ensure appropriate management and optimal patient outcomes.

Adapting the NIH Stroke Scale for Cognitive Impairment
When administering the NIH Stroke Scale on confused patients, it becomes imperative to adapt assessment techniques to accommodate cognitive impairment. Modifications may include simplifying instructions, providing additional cues, and adjusting scoring criteria to ensure accurate evaluation of neurological deficits amidst the confusion.
Importance of Accurate Assessment in Stroke Management
The NIH Stroke Scale serves as a cornerstone in stroke management, guiding treatment decisions and prognosticating outcomes. Accurate assessment of stroke severity, even in the presence of confusion, is essential for initiating timely interventions such as thrombolytic therapy or endovascular procedures, thereby optimizing patient care and minimizing disability.

Key Components of the NIH Stroke Scale Examination
The NIH Stroke Scale comprises various components assessing motor function, sensation, language, and visual fields. Understanding the nuances of each component is crucial for accurate evaluation in confused patients. Healthcare providers must meticulously assess and document each element to derive a comprehensive understanding of the patient's neurological status.

Strategies for Administering the NIH Stroke Scale on Confused Patients
Healthcare professionals must employ tailored strategies when administering the NIH Stroke Scale on confused patients. This may involve establishing rapport, providing reassurance, and utilizing non-verbal communication techniques to enhance patient cooperation and facilitate accurate assessment.
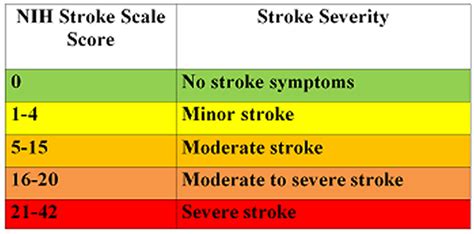
Interpreting NIH Stroke Scale Scores in the Context of Confusion
Interpretation of NIH Stroke Scale scores in confused patients requires astute clinical judgment and consideration of the underlying cognitive impairment. Healthcare providers must discern between deficits attributable to stroke and those influenced by confusion, ensuring accurate interpretation and subsequent management decisions.

Impact of Confusion on Stroke Treatment Decisions
Confusion can significantly impact stroke treatment decisions, potentially obscuring the delineation of stroke mimics or complicating the assessment of treatment eligibility criteria. Healthcare providers must navigate these challenges judiciously, prioritizing patient safety and optimal outcomes amidst the complexities presented by confusion.

Addressing Limitations and Pitfalls in NIH Stroke Scale Application
While the NIH Stroke Scale is a valuable tool, it is not without limitations. In the context of confusion, limitations may arise due to the inability to accurately assess certain components or interpret findings. Healthcare providers must remain cognizant of these pitfalls and exercise caution when applying the scale to ensure its efficacy in guiding clinical decisions.
Enhancing Clinical Practice: Integrating NIH Stroke Scale in Confused Patient Care
Integrating the NIH Stroke Scale into confused patient care necessitates a comprehensive understanding of both stroke assessment principles and cognitive impairment management strategies. By leveraging evidence-based practices and fostering interdisciplinary collaboration, healthcare providers can enhance clinical practice and optimize outcomes for confused patients presenting with stroke symptoms.
Sources:
1. Kim, B. J., Han, M. K., Park, T. H., Park, S. S., Lee, K. B., Lee, B. C., ... & Bae, H. J. (2014). Current status of acute stroke management in Korea: a report on a multicenter, comprehensive acute stroke registry. International Journal of Stroke, 9(4), 514-518.
2. Barber, P. A., Demchuk, A. M., Zhang, J., & Buchan, A. M. (2000). Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic
NIH Stroke Scale on Confused Patient in Professional's eye
The implementation of the
NIH Stroke Scale in evaluating
confused patients within healthcare settings underscores a critical intersection between neurological assessment and cognitive impairment management. Amidst the complexity inherent in such scenarios, healthcare professionals face multifaceted challenges that necessitate a nuanced approach. Adapting the NIH Stroke Scale for
cognitive impairment entails not only understanding the scale's components but also employing tailored strategies to ensure accurate evaluation. Despite the challenges posed by confusion, the importance of precise assessment cannot be overstated, as it informs treatment decisions and prognosticates outcomes. Interpreting NIH Stroke Scale scores in the context of confusion demands astute clinical judgment to distinguish between deficits attributable to stroke and those influenced by cognitive impairment. Moreover, addressing the limitations and pitfalls associated with the scale's application is paramount, safeguarding against erroneous interpretations and guiding effective patient management. Integrating the NIH Stroke Scale into clinical practice for confused patients requires a comprehensive understanding of both stroke assessment principles and cognitive impairment management strategies, fostering interdisciplinary collaboration to optimize patient care and outcomes.
Point of Views : NIH Stroke Scale on Confused Patient
The utilization of the
NIH Stroke Scale in assessing
confused patients within healthcare settings highlights the intricate balance between neurological evaluation and cognitive impairment management.Adapting the NIH Stroke Scale for
cognitive impairment necessitates a thorough understanding of its components and the implementation of tailored assessment strategies to ensure accuracy.The significance of precise assessment cannot be overstated, as it informs treatment decisions and prognosticates outcomes for
patients presenting with stroke symptoms amidst confusion.Interpreting NIH Stroke Scale scores in the context of confusion requires clinicians to exercise clinical judgment, discerning between deficits attributable to stroke and those influenced by cognitive impairment.Addressing the limitations and pitfalls associated with the scale's application is crucial, safeguarding against erroneous interpretations and guiding effective patient management.Integrating the NIH Stroke Scale into clinical practice for confused patients entails a comprehensive understanding of both stroke assessment principles and cognitive impairment management strategies, facilitating interdisciplinary collaboration to optimize patient care and outcomes.
Conclusion :As we conclude our exploration of the NIH Stroke Scale in the context of confused patients, it becomes evident that navigating the complexities of stroke assessment amidst cognitive impairment requires a meticulous and nuanced approach. Through our discussion, we have underscored the critical importance of accurate evaluation in guiding treatment decisions and prognosticating outcomes for patients presenting with stroke symptoms in the presence of confusion.
As healthcare professionals, it is incumbent upon us to continuously refine our understanding of the NIH Stroke Scale and its application in diverse clinical scenarios. By adapting assessment techniques and integrating interdisciplinary perspectives, we can enhance the quality of care provided to confused patients and optimize their chances of favorable outcomes. We trust that the insights shared in this series will serve as a valuable resource in your clinical practice, empowering you to navigate the intricacies of stroke assessment with confidence and proficiency.
Questions and Answer for NIH Stroke Scale on Confused Patient
Q: What is the NIH Stroke Scale?
- A: The NIH Stroke Scale is a standardized tool used by healthcare professionals to assess the severity of stroke symptoms in patients.
Q: How is the NIH Stroke Scale administered on confused patients?
- A: Administering the NIH Stroke Scale on confused patients requires adapting assessment techniques to accommodate cognitive impairment. This may involve simplifying instructions, providing additional cues, and adjusting scoring criteria for accurate evaluation.
Q: Why is accurate assessment important for confused patients?
- A: Accurate assessment is crucial for guiding treatment decisions and predicting outcomes in confused patients presenting with stroke symptoms. It ensures timely interventions and optimized patient care.
Q: What challenges are faced when using the NIH Stroke Scale on confused patients?
- A: Challenges include discerning between deficits attributable to stroke and those influenced by cognitive impairment, as well as addressing limitations in accurately assessing certain components of the scale.
Q: How can healthcare professionals enhance the application of the NIH Stroke Scale in confused patients?
- A: Healthcare professionals can enhance application by refining their understanding of stroke assessment principles, implementing tailored strategies for cognitive impairment management, and fostering interdisciplinary collaboration.
Label :NIH Stroke Scale, Confused PatientsHealthcare, Assessment Techniques
Keyword : NIH Stroke Scale on Confused Patient
0 komentar