Unlocking Stroke Severity: Decoding the Modified NIH Stroke Scale
Discover the invaluable insights of the Modified NIH Stroke Scale (mNIHSS) and elevate your understanding of stroke assessment for enhanced patient care.
In the realm of stroke assessment, the Modified NIH Stroke Scale (mNIHSS) stands as a critical tool, guiding healthcare professionals in evaluating the severity of stroke-related impairments. Amidst the intricate landscape of healthcare, understanding the nuances of stroke assessment is paramount. This article delves into the intricacies of the mNIHSS, elucidating its significance in clinical practice and its role in informing treatment decisions. As we embark on this journey, let us navigate through the complexities of stroke evaluation, unraveling the essence of the mNIHSS and its implications for patient care.
Top 10 Points about Modified NIH Stroke Scale :
- The Evolution of Stroke Assessment: Introducing the Modified NIH Stroke Scale
- Understanding the Components of the mNIHSS: A Comprehensive Overview
- Interpreting Neurological Deficits: Insights from the mNIHSS
- Scoring Stroke Severity: Utilizing the mNIHSS in Clinical Practice
- Assessing Consciousness and Language Function with the mNIHSS
- Exploring Motor Function Assessment: The Role of the mNIHSS
- Facial Palsy Evaluation: Insights from the Modified NIH Stroke Scale
- Unraveling Sensory Impairments: An Examination Through the mNIHSS Lens
- Crucial Role of the mNIHSS in Treatment Decision Making for Stroke Patients
- Enhancing Patient Outcomes: Optimizing Stroke Management with the mNIHSS
Several facts about Modified NIH Stroke Scale

Introduction
In the realm of stroke assessment, healthcare professionals rely on standardized tools to evaluate the severity of neurological deficits in patients. One such tool that plays a pivotal role in this domain is the Modified NIH Stroke Scale (mNIHSS). Developed as an adaptation of the National Institutes of Health Stroke Scale (NIHSS), the mNIHSS offers a structured approach to assessing stroke-related impairments, aiding in treatment decision-making and prognosis determination.

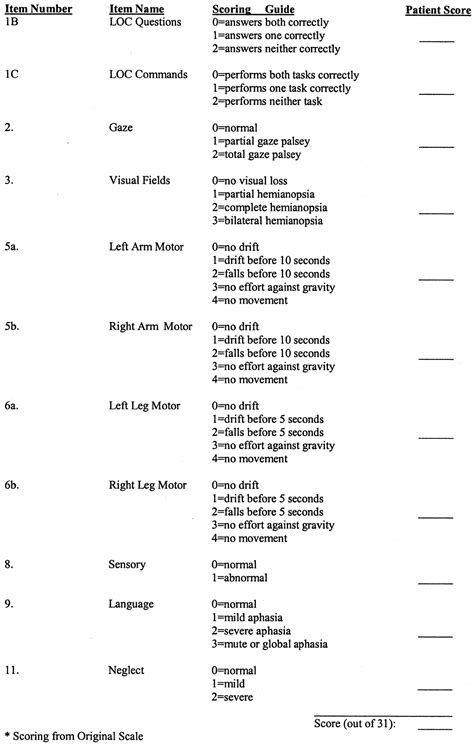
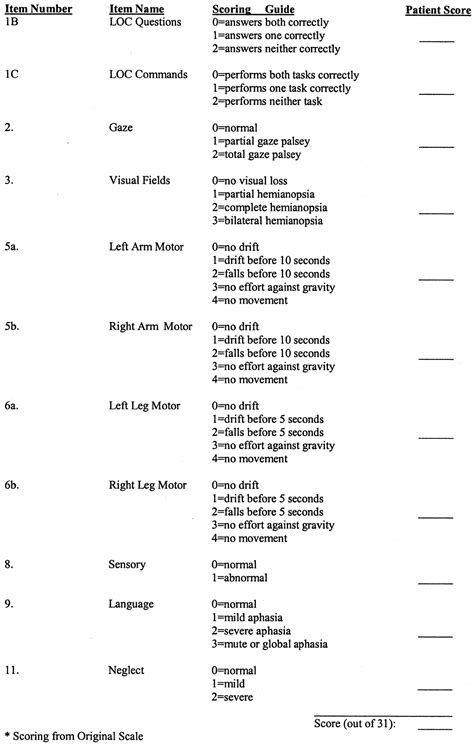
Components of the mNIHSS
The mNIHSS comprises various components, each meticulously designed to assess specific aspects of neurological function. These components include evaluations of consciousness, language, motor function, visual fields, facial palsy, motor arm and leg, limb ataxia, sensory, and neglect. Through a comprehensive examination of these domains, healthcare providers can gain valuable insights into the extent and nature of a patient's stroke-related deficits.

Interpreting Neurological Deficits
Interpreting the results of the mNIHSS requires a nuanced understanding of neurological deficits and their implications for patient outcomes. Each component of the scale provides crucial information about the location and severity of the stroke, guiding healthcare professionals in developing tailored treatment plans. By carefully analyzing the findings of the mNIHSS, clinicians can identify areas of impairment and prioritize interventions to optimize patient recovery.

Scoring Stroke Severity
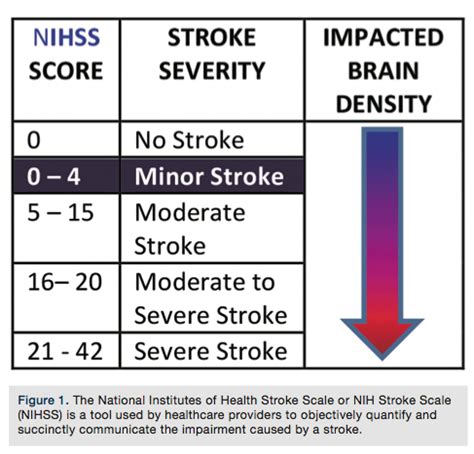
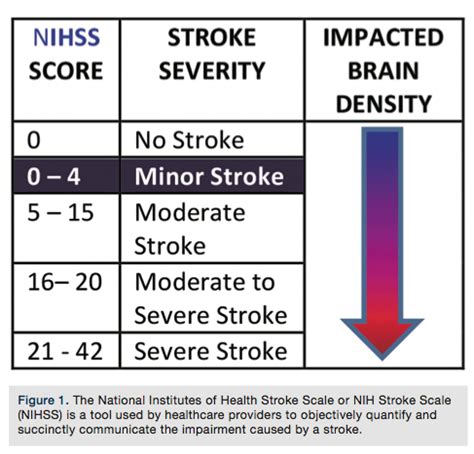
The mNIHSS assigns scores to each component based on the severity of impairment observed during assessment. These scores range from 0 (indicating no impairment) to 4 (indicating severe impairment). By summing the scores across all components, healthcare providers can quantify the overall severity of the stroke. This standardized scoring system facilitates communication among multidisciplinary teams and enables consistent monitoring of patients' progress over time.

Assessing Consciousness and Language Function
Two critical components of the mNIHSS focus on assessing consciousness and language function, both of which are commonly affected by stroke. Consciousness evaluation involves assessing the patient's level of alertness and responsiveness to stimuli, providing insights into the overall severity of the neurological insult. Language function assessment, on the other hand, evaluates the patient's ability to comprehend and produce speech, offering valuable information about potential aphasia or dysarthria.

Exploring Motor Function Assessment
The motor function assessment component of the mNIHSS encompasses evaluations of motor strength in the upper and lower extremities, as well as assessments of limb ataxia and facial symmetry. By systematically examining motor function, healthcare providers can identify hemiparesis or hemiplegia, assess for signs of motor coordination deficits, and monitor for the presence of facial droop—a common indicator of stroke.

Facial Palsy Evaluation
Facial palsy evaluation is a crucial aspect of the mNIHSS that focuses on assessing asymmetry of facial movements, particularly in the presence of a suspected stroke affecting the facial nerve. By observing the patient's ability to smile, close their eyes tightly, and raise their eyebrows, healthcare providers can discern the presence and severity of facial weakness—a hallmark feature of certain types of stroke.

Unraveling Sensory Impairments
Sensory assessment is integral to the mNIHSS and involves evaluating the patient's ability to perceive light touch and proprioceptive stimuli on both sides of the body. By meticulously assessing sensory function, healthcare providers can detect sensory deficits that may accompany motor impairments, providing valuable insights into the extent and distribution of neurological damage.
Crucial Role of the mNIHSS in Treatment Decision Making
The mNIHSS plays a pivotal role in guiding treatment decision-making for patients with acute stroke. By accurately assessing the severity of neurological deficits, healthcare providers can determine the most appropriate course of action, which may include thrombolytic therapy, endovascular intervention, or supportive care measures. The timely and accurate application of the mNIHSS can significantly impact patient outcomes and improve overall prognosis.

Enhancing Patient Outcomes
By incorporating the mNIHSS into routine clinical practice, healthcare providers can enhance patient outcomes through optimized stroke management. The systematic assessment of neurological deficits, coupled with the accurate quantification of stroke severity, enables targeted interventions aimed at minimizing disability and promoting recovery. Ultimately, the mNIHSS serves as a valuable tool in the comprehensive care of patients with stroke, facilitating evidence-based decision-making and improving quality of life.
Sources:
1. National Institute of Neurological
Modified NIH Stroke Scale in Professional's eye
In the realm of healthcare, the
Modified NIH Stroke Scale (mNIHSS) stands as a cornerstone in the assessment and management of stroke, offering a standardized approach to evaluating the severity of neurological deficits in affected individuals. As an adaptation of the National Institutes of Health Stroke Scale (NIHSS), the
mNIHSS serves as a comprehensive tool for healthcare professionals to quantify and monitor the impact of stroke on patients' neurological function. This scale encompasses various components, each meticulously designed to assess specific domains such as consciousness, language, motor function, and sensory perception. Through a systematic evaluation of these domains, clinicians can gain valuable insights into the location and extent of neurological damage, facilitating timely and targeted interventions. The
mNIHSS not only aids in the initial assessment of stroke severity but also plays a crucial role in treatment decision-making and prognostication. By assigning scores to each component based on the severity of impairment observed, healthcare providers can objectively quantify the overall severity of the stroke and tailor treatment strategies accordingly. Additionally, the
mNIHSS serves as a valuable tool for monitoring patients' progress over time, allowing clinicians to adjust treatment plans as needed and assess the effectiveness of interventions. Moreover, the standardized nature of the
mNIHSS facilitates communication among multidisciplinary healthcare teams, ensuring consistent and coordinated care for stroke patients across various clinical settings. Through its systematic approach to stroke assessment, the
mNIHSS contributes to improved patient outcomes by guiding evidence-based interventions and optimizing the delivery of care.
Point of Views : Modified NIH Stroke Scale
Utilize the
Modified NIH Stroke Scale (mNIHSS) as a standardized tool for assessing stroke severity in patients presenting with neurological deficits.Familiarize oneself with the components of the
mNIHSS, including assessments of consciousness, language function, motor strength, sensory perception, and other relevant domains.Administer the
mNIHSS according to established protocols and guidelines, ensuring consistency and accuracy in scoring.Document the scores obtained for each component of the
mNIHSS meticulously, as these scores serve as objective measures of stroke severity and guide treatment decisions.Collaborate with interdisciplinary healthcare teams to interpret the results of the
mNIHSS and develop individualized treatment plans for stroke patients.Monitor patients' progress over time by repeating the
mNIHSS assessment at regular intervals, allowing for adjustments to treatment strategies as needed.Communicate effectively with patients and their families about the implications of the
mNIHSS scores and the prognosis for recovery.Continuously update one's knowledge and skills in administering and interpreting the
mNIHSS through ongoing education and training opportunities.Advocate for the widespread use of the
mNIHSS in healthcare settings to ensure standardized and comprehensive assessment of stroke severity across diverse patient populations.
Conclusion :As we conclude our exploration of the Modified NIH Stroke Scale (mNIHSS) and its significance in healthcare, it's essential to reflect on the invaluable insights gained from our discussion. Through a comprehensive analysis of the components and applications of the mNIHSS, we've elucidated its critical role in assessing stroke severity and guiding treatment decisions. By utilizing this standardized tool, healthcare professionals can accurately quantify the neurological deficits associated with stroke and tailor interventions to optimize patient outcomes.
Moreover, the widespread adoption of the mNIHSS in clinical practice underscores its relevance and utility in the management of stroke patients. As we continue to strive for excellence in stroke care, let us remain committed to leveraging the mNIHSS as a cornerstone of our assessment and treatment protocols. Together, we can ensure that every stroke patient receives the comprehensive and personalized care they deserve, ultimately improving their chances of recovery and enhancing their quality of life.
Questions and Answer for Modified NIH Stroke Scale
When discussing the Modified NIH Stroke Scale (mNIHSS), people often have several common questions. Here are some of the frequently asked questions along with their answers:
- 1. What is the purpose of the Modified NIH Stroke Scale?
The mNIHSS is a standardized tool used by healthcare professionals to assess the severity of neurological deficits in patients who have experienced a stroke. It helps in quantifying the extent of impairment across various domains such as consciousness, language, motor function, and sensory perception.
- 2. How is the Modified NIH Stroke Scale administered?
The mNIHSS is administered by trained healthcare providers who systematically evaluate the patient's neurological function based on a series of standardized tasks and questions. Each component is scored based on the severity of impairment observed, with higher scores indicating more severe deficits.
- 3. What information does the Modified NIH Stroke Scale provide?
The mNIHSS provides valuable information about the location and severity of neurological damage resulting from a stroke. It helps healthcare providers in making treatment decisions, predicting prognosis, and monitoring patients' progress over time.
- 4. Is the Modified NIH Stroke Scale suitable for all types of strokes?
While the mNIHSS is widely used for assessing the severity of ischemic strokes, it may not be as effective for certain types of hemorrhagic strokes or other neurological conditions. Healthcare providers may need to use additional assessment tools or modify the mNIHSS protocol accordingly in such cases.
- 5. How does the Modified NIH Stroke Scale compare to other stroke assessment tools?
The mNIHSS is one of the most commonly used stroke assessment tools due to its standardized nature and comprehensive evaluation of neurological function. However, other scales such as the Glasgow Coma Scale (GCS) and the Canadian Neurological Scale (CNS) may also be used depending on the clinical context and patient population.
Label :Modified NIH Stroke Scale, Healthcare Assessment, Stroke Severity
Keyword : Modified NIH Stroke Scale
Discover the invaluable insights of the Modified NIH Stroke Scale (mNIHSS) and elevate your understanding of stroke assessment for enhanced patient care.
In the realm of stroke assessment, the Modified NIH Stroke Scale (mNIHSS) stands as a critical tool, guiding healthcare professionals in evaluating the severity of stroke-related impairments. Amidst the intricate landscape of healthcare, understanding the nuances of stroke assessment is paramount. This article delves into the intricacies of the mNIHSS, elucidating its significance in clinical practice and its role in informing treatment decisions. As we embark on this journey, let us navigate through the complexities of stroke evaluation, unraveling the essence of the mNIHSS and its implications for patient care.
Top 10 Points about Modified NIH Stroke Scale :
- The Evolution of Stroke Assessment: Introducing the Modified NIH Stroke Scale
- Understanding the Components of the mNIHSS: A Comprehensive Overview
- Interpreting Neurological Deficits: Insights from the mNIHSS
- Scoring Stroke Severity: Utilizing the mNIHSS in Clinical Practice
- Assessing Consciousness and Language Function with the mNIHSS
- Exploring Motor Function Assessment: The Role of the mNIHSS
- Facial Palsy Evaluation: Insights from the Modified NIH Stroke Scale
- Unraveling Sensory Impairments: An Examination Through the mNIHSS Lens
- Crucial Role of the mNIHSS in Treatment Decision Making for Stroke Patients
- Enhancing Patient Outcomes: Optimizing Stroke Management with the mNIHSS
Several facts about Modified NIH Stroke Scale

Introduction
In the realm of stroke assessment, healthcare professionals rely on standardized tools to evaluate the severity of neurological deficits in patients. One such tool that plays a pivotal role in this domain is the Modified NIH Stroke Scale (mNIHSS). Developed as an adaptation of the National Institutes of Health Stroke Scale (NIHSS), the mNIHSS offers a structured approach to assessing stroke-related impairments, aiding in treatment decision-making and prognosis determination.

Components of the mNIHSS
The mNIHSS comprises various components, each meticulously designed to assess specific aspects of neurological function. These components include evaluations of consciousness, language, motor function, visual fields, facial palsy, motor arm and leg, limb ataxia, sensory, and neglect. Through a comprehensive examination of these domains, healthcare providers can gain valuable insights into the extent and nature of a patient's stroke-related deficits.

Interpreting Neurological Deficits
Interpreting the results of the mNIHSS requires a nuanced understanding of neurological deficits and their implications for patient outcomes. Each component of the scale provides crucial information about the location and severity of the stroke, guiding healthcare professionals in developing tailored treatment plans. By carefully analyzing the findings of the mNIHSS, clinicians can identify areas of impairment and prioritize interventions to optimize patient recovery.

Scoring Stroke Severity
The mNIHSS assigns scores to each component based on the severity of impairment observed during assessment. These scores range from 0 (indicating no impairment) to 4 (indicating severe impairment). By summing the scores across all components, healthcare providers can quantify the overall severity of the stroke. This standardized scoring system facilitates communication among multidisciplinary teams and enables consistent monitoring of patients' progress over time.

Assessing Consciousness and Language Function
Two critical components of the mNIHSS focus on assessing consciousness and language function, both of which are commonly affected by stroke. Consciousness evaluation involves assessing the patient's level of alertness and responsiveness to stimuli, providing insights into the overall severity of the neurological insult. Language function assessment, on the other hand, evaluates the patient's ability to comprehend and produce speech, offering valuable information about potential aphasia or dysarthria.

Exploring Motor Function Assessment
The motor function assessment component of the mNIHSS encompasses evaluations of motor strength in the upper and lower extremities, as well as assessments of limb ataxia and facial symmetry. By systematically examining motor function, healthcare providers can identify hemiparesis or hemiplegia, assess for signs of motor coordination deficits, and monitor for the presence of facial droop—a common indicator of stroke.

Facial Palsy Evaluation
Facial palsy evaluation is a crucial aspect of the mNIHSS that focuses on assessing asymmetry of facial movements, particularly in the presence of a suspected stroke affecting the facial nerve. By observing the patient's ability to smile, close their eyes tightly, and raise their eyebrows, healthcare providers can discern the presence and severity of facial weakness—a hallmark feature of certain types of stroke.

Unraveling Sensory Impairments
Sensory assessment is integral to the mNIHSS and involves evaluating the patient's ability to perceive light touch and proprioceptive stimuli on both sides of the body. By meticulously assessing sensory function, healthcare providers can detect sensory deficits that may accompany motor impairments, providing valuable insights into the extent and distribution of neurological damage.
Crucial Role of the mNIHSS in Treatment Decision Making
The mNIHSS plays a pivotal role in guiding treatment decision-making for patients with acute stroke. By accurately assessing the severity of neurological deficits, healthcare providers can determine the most appropriate course of action, which may include thrombolytic therapy, endovascular intervention, or supportive care measures. The timely and accurate application of the mNIHSS can significantly impact patient outcomes and improve overall prognosis.

Enhancing Patient Outcomes
By incorporating the mNIHSS into routine clinical practice, healthcare providers can enhance patient outcomes through optimized stroke management. The systematic assessment of neurological deficits, coupled with the accurate quantification of stroke severity, enables targeted interventions aimed at minimizing disability and promoting recovery. Ultimately, the mNIHSS serves as a valuable tool in the comprehensive care of patients with stroke, facilitating evidence-based decision-making and improving quality of life.
Sources:
1. National Institute of Neurological
Modified NIH Stroke Scale in Professional's eye
In the realm of healthcare, the
Modified NIH Stroke Scale (mNIHSS) stands as a cornerstone in the assessment and management of stroke, offering a standardized approach to evaluating the severity of neurological deficits in affected individuals. As an adaptation of the National Institutes of Health Stroke Scale (NIHSS), the
mNIHSS serves as a comprehensive tool for healthcare professionals to quantify and monitor the impact of stroke on patients' neurological function. This scale encompasses various components, each meticulously designed to assess specific domains such as consciousness, language, motor function, and sensory perception. Through a systematic evaluation of these domains, clinicians can gain valuable insights into the location and extent of neurological damage, facilitating timely and targeted interventions. The
mNIHSS not only aids in the initial assessment of stroke severity but also plays a crucial role in treatment decision-making and prognostication. By assigning scores to each component based on the severity of impairment observed, healthcare providers can objectively quantify the overall severity of the stroke and tailor treatment strategies accordingly. Additionally, the
mNIHSS serves as a valuable tool for monitoring patients' progress over time, allowing clinicians to adjust treatment plans as needed and assess the effectiveness of interventions. Moreover, the standardized nature of the
mNIHSS facilitates communication among multidisciplinary healthcare teams, ensuring consistent and coordinated care for stroke patients across various clinical settings. Through its systematic approach to stroke assessment, the
mNIHSS contributes to improved patient outcomes by guiding evidence-based interventions and optimizing the delivery of care.
Point of Views : Modified NIH Stroke Scale
Utilize the
Modified NIH Stroke Scale (mNIHSS) as a standardized tool for assessing stroke severity in patients presenting with neurological deficits.Familiarize oneself with the components of the
mNIHSS, including assessments of consciousness, language function, motor strength, sensory perception, and other relevant domains.Administer the
mNIHSS according to established protocols and guidelines, ensuring consistency and accuracy in scoring.Document the scores obtained for each component of the
mNIHSS meticulously, as these scores serve as objective measures of stroke severity and guide treatment decisions.Collaborate with interdisciplinary healthcare teams to interpret the results of the
mNIHSS and develop individualized treatment plans for stroke patients.Monitor patients' progress over time by repeating the
mNIHSS assessment at regular intervals, allowing for adjustments to treatment strategies as needed.Communicate effectively with patients and their families about the implications of the
mNIHSS scores and the prognosis for recovery.Continuously update one's knowledge and skills in administering and interpreting the
mNIHSS through ongoing education and training opportunities.Advocate for the widespread use of the
mNIHSS in healthcare settings to ensure standardized and comprehensive assessment of stroke severity across diverse patient populations.
Conclusion :As we conclude our exploration of the Modified NIH Stroke Scale (mNIHSS) and its significance in healthcare, it's essential to reflect on the invaluable insights gained from our discussion. Through a comprehensive analysis of the components and applications of the mNIHSS, we've elucidated its critical role in assessing stroke severity and guiding treatment decisions. By utilizing this standardized tool, healthcare professionals can accurately quantify the neurological deficits associated with stroke and tailor interventions to optimize patient outcomes.
Moreover, the widespread adoption of the mNIHSS in clinical practice underscores its relevance and utility in the management of stroke patients. As we continue to strive for excellence in stroke care, let us remain committed to leveraging the mNIHSS as a cornerstone of our assessment and treatment protocols. Together, we can ensure that every stroke patient receives the comprehensive and personalized care they deserve, ultimately improving their chances of recovery and enhancing their quality of life.
Questions and Answer for Modified NIH Stroke Scale
When discussing the Modified NIH Stroke Scale (mNIHSS), people often have several common questions. Here are some of the frequently asked questions along with their answers:
- 1. What is the purpose of the Modified NIH Stroke Scale?
The mNIHSS is a standardized tool used by healthcare professionals to assess the severity of neurological deficits in patients who have experienced a stroke. It helps in quantifying the extent of impairment across various domains such as consciousness, language, motor function, and sensory perception.
- 2. How is the Modified NIH Stroke Scale administered?
The mNIHSS is administered by trained healthcare providers who systematically evaluate the patient's neurological function based on a series of standardized tasks and questions. Each component is scored based on the severity of impairment observed, with higher scores indicating more severe deficits.
- 3. What information does the Modified NIH Stroke Scale provide?
The mNIHSS provides valuable information about the location and severity of neurological damage resulting from a stroke. It helps healthcare providers in making treatment decisions, predicting prognosis, and monitoring patients' progress over time.
- 4. Is the Modified NIH Stroke Scale suitable for all types of strokes?
While the mNIHSS is widely used for assessing the severity of ischemic strokes, it may not be as effective for certain types of hemorrhagic strokes or other neurological conditions. Healthcare providers may need to use additional assessment tools or modify the mNIHSS protocol accordingly in such cases.
- 5. How does the Modified NIH Stroke Scale compare to other stroke assessment tools?
The mNIHSS is one of the most commonly used stroke assessment tools due to its standardized nature and comprehensive evaluation of neurological function. However, other scales such as the Glasgow Coma Scale (GCS) and the Canadian Neurological Scale (CNS) may also be used depending on the clinical context and patient population.
Label :Modified NIH Stroke Scale, Healthcare Assessment, Stroke Severity
Keyword : Modified NIH Stroke Scale
0 komentar